The Role of Mobile Health Applications for Medical Decision Support: A Literature Review
Abstract
Objectives:
Methods:
Results:
Conclusion:
Introduction
Smartphones, hand-held, wearable and non-wearable devices and mHealth applications have become common tools used by people in today’s life. Statista’s The Statistical Portal estimated that the number of mobile phone users will raise to 4.93 billion at the end of 2018, which is also expected to reach 5.07 billion by the end of 2019 (Statista, 2018). Some researchers argue that these tools play an important role in the way people manage their daily life including their healthcare (Wang, Xiang, & Fesenmaier, 2016). More specifically, the introduction of mHealth gadgets and applications enabled people to search information on their medical conditions and seek advices to manage such conditions (Sarwar & Soomro, 2013). However, some medical practitioners raise their concerns regarding the authenticity of medical information provided through these applications and health information websites (Kaneez & Hassan, 2015).
Kay, Santos, and Takane (2011)defined mobile health (mHealth) as clinical and public health services provided via mobile phones and wireless-hand held electronic devices. These tools or devices are known as easy to use, connected to the Internet, and can have the ability to provide a wide range of health information and services for their users. mHealth applications are growing in numbers, which reached to 165,000 in 2018 (Lang & Zawati, 2018). They also explained that these applications are available for people to use them at any time to search health related data and seek advices for their concerns in an interactive way. Lang and Zawati (2018) highlighted that these applications may also empower patients in making medical decisions including increase of their awareness about symptoms, diagnosis and some management instructions.
Medical specialities and sub-specialties are increasing remarkably, it is challenging for doctors to keep with the advance medical knowledge. Continuous medical education programmes, conferences and seminars are the way that help doctors update their medical knowledge, which requires plenty of time from their busy schedule (MacWalter, McKay, & Bowie, 2016). O'Donovan, Bersin, and O'Donovan (2015) stated that mHealth applications can provide clinicians diagnosis of specific conditions, differential diagnosis, investigation protocols and can help doctors predict outcome of management plans using interactive data entrance. The literature here suggests that mHealth can offer a platform for doctors to keep up with the advance medical knowledge. These tools also can help doctors make evidence-based medical decisions adhered to guidelines and protocols, and allow them to engage in discussions, share thoughts and views with colleagues and experts in specific speciality areas.
With the growing number of mHealth application and its influence on clinical practice, researchers however, raise concerns regarding the reliability and validity of these tools and how that could impact on consumers’ management of their own healthcare conditions (Abbasgholizadeh Rahimi, Menear, Robitaille, & Légaré, 2017). Absence of unified standards and guidelines in the development of mHealth application, authenticity of its medical content and privacy of consumers’ data are some issues raised by researchers in this respect. However, some experts are overly optimistic about mHealth applications considering them as the future of the healthcare. Steinhubl, Muse, and Topol (2015) believe that these applications are encompassed with the ability of machine learning and features of artificial intelligence, which can revolutionise the way healthcare is provided and received. Examining the selected literature, the paper aims to understand the role of mHealth applications in supporting medical decision for both healthcare providers and patients.
Methods
Literature search was conducted from NCBI PubMed and Google Scholar websites that were published from January 2014 to April 2018, as seen in Figure 1. Table 1 shows the keywords used to search articles and the inclusion criteria applied for the selection of articles. The total number of papers returned through the literature search was 96 articles. While checking through the retrieved articles, three articles were found without abstracts and they were excluded. With the remained 93 articles, specific inclusion and exclusion criteria were applied (Table1) and 45 articles were selected for the examination to understand the role of mHealth applications that support medical decisions for both healthcare providers and patients. Using a literature matrix (Appendix 1), the articles were categorised based on specific areas of medical decision support for clinicians, outlining four themes that explained the role of mHealth application in medical decision support.
Table 1. Search terms and Inclusion criteria
|
Filters |
Inclusion criteria |
|
Search Keywords |
mobile AND health AND medical AND decision AND support. |
|
Main headings |
Mobile health applications or software that support medical decision making for medical professionals and patients. This excludes other software platforms those are fixed at medical service providing stations. |
|
Study design |
Original study that evaluates mHealth application specifically designed to support medical decision making. Literature reviews, and those did not evaluate applications are excluded. |
|
Language |
Only articles written in English are included. |
|
Time-period |
Articles published last 5 years are included (2014 to 2018). |
Figure 1 shows the flowchart of search and the selection process of articles for this literature review. The selected articles are then reviewed and categorised according to specific areas of medical decision support, identifying four themes that explained the role of mHealth application in medical decision support.
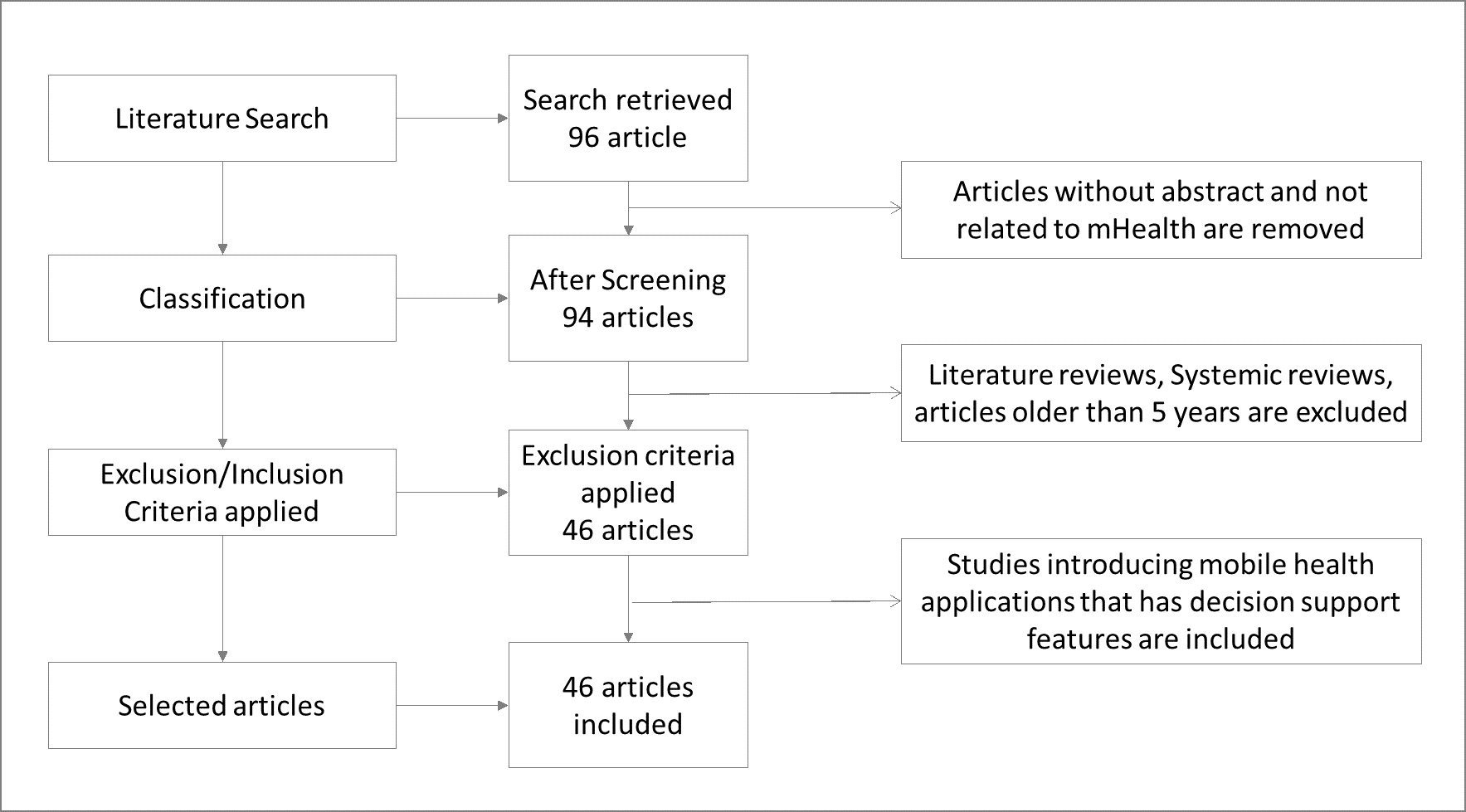
Figure 1.Search and selection process of articles
Results
Articles that met the inclusion criteria are categorised according to specific areas of medical decision support for clinicians. The literature matrix (Appendix 1) illustrates the selected articles, their main themes, outcomes and application targeted areas. Table 2 shows main categories and the number of articles that introduced mobile application, which support medical decision making. Table 2 also illustrates that mHealth applications to decision support for healthcare providers represented a large percent of applications with 68.8%, followed by 28.8%, which represented the decision support for both healthcare providers and patients. It also highlights that mHealth applications supported for medical decisions only for patients are limited, which represented 2.2%.
Table 1.Selected articles categorized
|
Categories |
Number |
Percentage |
|---|---|---|
|
Decision support for health care providers |
31 |
68.8% |
|
Decision support for Patients |
1 |
2.2% |
|
Decision support for Health care providers and Patients |
13 |
28.8% |
|
Application for cardio vascular diseases |
6 |
13.3% |
|
Application for Antimicrobial therapies |
2 |
4.4% |
|
Application for Laboratory investigation request |
1 |
2.2% |
|
Application for neonatal and maternal health |
2 |
4.4% |
|
Application for Experience sampling method |
1 |
2.2% |
|
Application for stroke prevention |
1 |
2.2% |
|
Application for mental health |
3 |
6.6% |
|
Application for Ophthalmologists |
1 |
2.2% |
|
Application for food environment assessment |
1 |
2.2% |
|
Application for Parkinson's disease |
2 |
4.4% |
|
Application for Family health data collection |
1 |
2.2% |
|
Application to detect delirium |
1 |
2.2% |
|
Application to support paediatric drug mixing |
1 |
2.2% |
|
Application to support sepsis control |
2 |
4.4% |
|
Application to support rural health |
2 |
4.4% |
|
Application to decision support on diabetic patients |
3 |
6.6% |
|
Application for Burn injuries |
1 |
2.2% |
|
Application for remote monitoring of elders |
2 |
4.4% |
|
Application for Emergency checklist (Paramedics) |
2 |
4.4% |
|
Application for End Stage Renal Failure decision support |
1 |
2.2% |
|
Application for Bronchial asthma |
1 |
2.2% |
|
Application for pre-hospital care of trauma patients |
2 |
4.4% |
|
Application for medical decision support for junior doctors |
2 |
4.4% |
|
Application for medical data visualisation to assist in decision support |
1 |
2.2% |
|
Application for Hemotherapy decision support |
1 |
2.2% |
Table 2 illustrates that mHealth applications were targeted to support decision making in various areas of medical field. Developers of mHealth applications covered 25 different areas of medical field. The highest number of applications focused on Cardio Vascular Diseases (CVD), as it reached to 13.3%. The second common area is Diabetes represented 6.6% of all applications. The other important areas covered by mHealth applications included Neonatal and Maternal Health, Mental Health, Anti-microbial therapy decision making, Sepsis control, Parkinson’s Disease (see Table 2). Figure 2 shows the distribution of number of applications over five years, the highest number of applications were (14) introduced during 2015, while the lowest (2) included in this review was in 2018, as the literature search was conducted up until May 2018. Synthesising the literature, the paper identified four themes, as discussed in the following sections.
Table 1.Selected articles categorised
|
Categories |
Number |
Percentage |
|---|---|---|
|
Decision support for health care providers |
31 |
68.8% |
|
Decision support for Patients |
1 |
2.2% |
|
Decision support for Health care providers and Patients |
13 |
28.8% |
|
Application for cardio vascular diseases |
6 |
13.3% |
|
Application for Antimicrobial therapies |
2 |
4.4% |
|
Application for Laboratory investigation request |
1 |
2.2% |
|
Application for neonatal and maternal health |
2 |
4.4% |
|
Application for Experience sampling method |
1 |
2.2% |
|
Application for stroke prevention |
1 |
2.2% |
|
Application for mental health |
3 |
6.6% |
|
Application for Ophthalmologists |
1 |
2.2% |
|
Application for food environment assessment |
1 |
2.2% |
|
Application for Parkinson's disease |
2 |
4.4% |
|
Application for Family health data collection |
1 |
2.2% |
|
Application to detect delirium |
1 |
2.2% |
|
Application to support paediatric drug mixing |
1 |
2.2% |
|
Application to support sepsis control |
2 |
4.4% |
|
Application to support rural health |
2 |
4.4% |
|
Application to decision support on diabetic patients |
3 |
6.6% |
|
Application for Burn injuries |
1 |
2.2% |
|
Application for remote monitoring of elders |
2 |
4.4% |
|
Application for Emergency checklist (Paramedics) |
2 |
4.4% |
|
Application for End Stage Renal Failure decision support |
1 |
2.2% |
|
Application for Bronchial asthma |
1 |
2.2% |
|
Application for pre-hospital care of trauma patients |
2 |
4.4% |
|
Application for medical decision support for junior doctors |
2 |
4.4% |
|
Application for medical data visualisation to assist in decision support |
1 |
2.2% |
|
Application for Hemotherapy decision support |
1 |
2.2% |
Table 2 illustrates that mHealth applications were targeted to support decision making in various areas of medical field. Developers of mHealth applications covered 25 different areas of medical field. The highest number of applications focused on Cardio Vascular Diseases (CVD), as it reached to 13.3%. The second common area is Diabetes represented 6.6% of all applications. The other important areas covered by mHealth applications included Neonatal and Maternal Health, Mental Health, Anti-microbial therapy decision making, Sepsis control, Parkinson’s Disease (see Table 2). Figure 2 shows the distribution of number of applications over five years, the highest number of applications were (14) introduced during 2015, while the lowest (2) included in this review was in 2018, as the literature search was conducted up until May 2018. Synthesising the literature, the paper identified four themes, as discussed in the following sections.
.jpg)
Figure 2.Number of mHealth applications developed during the selected period
Discussion
The examined literature identified thought-provoking trends related to use of mHealth applications that support medical decision making. Important themes related to the role of mHealth applications to medical decision support are identified, as shown in Figure 3 and discussed below.
Figure 3. The role of mHealth Applications for medical decision support
mHealth Applications as a Medical Decision Supporter for Healthcare Providers
Ventola (2014)identified five categories that medical professionals use for different purposes: administration, health maintenance and access, communication and consultation, reference and information gathering, and medical education. Information gathering, and medical education are two common uses of mHealth applications by professionals, as the number of mHealth applications are increasing and it covers large number of medical specialities. Dicianno et al. (2015) asserted that clinician-oriented applications are useful for medical professionals, 1) as these applications provide them reference and educational materials, and 2) these applications assist them in clinical decision making by providing up-to date guidelines. The literature reviewed confirms this idea, as it showed more than two third of the applications are targeted to assist healthcare providers in their decision support.
There are several ways, in which mHealth applications can assist in medical decision making. For example, some application developers provided reference and educational material and patient involvement strategies (Charani et al., 2017; Guo et al., 2017; Manaktala & Claypool, 2017), protocols and algorithms for diagnosis with differential diagnosis of confusing medical conditions as mental disorders (Maulik et al., 2017; Yang et al., 2016), others provided patient evaluation and management tool kits as diabetic control, neonatal with maternal follow up tools and long distance monitoring of older adult tools (Bakibinga, Kamande, Omuya, Ziraba, & Kyobutungi, 2017; Bansal et al., 2015; Lamprinos et al., 2016). These are evidenced-based examples of using mHealth application for clinical decision support by healthcare providers. However, some experts argue that some mHealth applications did not meet the level of authenticity, confidentiality, reliability and user-friendliness encompassed within these tools (Yasini & Marchand, 2015). Issue of privacy breach with exposure of patient-related health data is a prominent concern among the consumers of mobile applications (Albuquerque & Gondim, 2016).
mHealth Applications as Empowering tools for Patients
Health conditions-related decision making is a critical issue that may have long lasting effect on someone’s life. Decision making from patient side does not always depend on adequate knowledge of the condition, possible outcomes and expected adverse events (Joseph-Williams, Elwyn, & Edwards, 2014). As a receiver of the health care, patients tend rely on information provided and explained by healthcare providers. With the introduction of mHealth applications, patients are offered ways to take informed decision about their medical conditions (Bradway, Årsand, & Grøttland, 2015). With the information patients receive from mHealth application, they are empowered and offered opportutnies to participate actively in making decision regarding their health conditions. Some of these examples are discussed in the literature such as patient-focused blood sugar control for Type 2 diabetes (Lloyd, Groat, Cook, Kaufman, & Grando, 2015), decision-support for breast cancer patients (Pezzin, Laud, Neuner, Yen, & Nattinger, 2016) and end-stage renal failure patients for decision to continue doing dialysis or decide on renal transplant (Patzer et al., 2016).
However, some researchers would argue that information received by patients through mHealth application could create more complex issues for healthcare professionals (Elwyn et al., 2012; Légaré & Witteman, 2013). Clinical scenarios and advices received via these applications and health websites may have different perspectives that has nothing to do with the authentic clinical knowledge. In such cases, healthcare providers may find it difficult to convince patients to follow their standard medical advices (Légaré et al., 2014). Such issues could be solved with continuous monitoring of standard guidelines of the content included in mHealth applications.
mHealth Applications as a Platform to Update Medical Knowledge
With ongoing research and advance medical knowledge, standard guidelines for management of medical conditions are remarkably changing in its content. This rapidly changing and updating of medical knowledge could lead to a knowledge-gap in medical practitioners’ up-to-date medical knowledge and standard protocols (Trevisonno et al., 2015). The examination of literature suggests that one way to maintain medical practitioners’ update of their knowledge is using mHealth applications. Recent advances of medical knowledge, research evidence-based findings, continuous educations programs, seminars can be provided through these applications. Such programmes can help medical practitioners reflect on their management of medical conditions. This ‘in turn’ can reduce the cost the number of unnecessary deviations from standard investigations and management pathways (Tshiamo, Kgositau, & Magowe, 2017). Literature selected for this paper identified some examples of mHealth applications that promote following the evidence-based medical management. Hagberg et al. (2016) developed mHealth application that guided medical practitioners in paediatric drug doses and drug mixing with evidence- based standard guidelines. The study found that the application reduced the number of adverse events in paediatric dose management. Similarly, Menezes and Gusmao (2015) developed mobile application that provided standard guidelines in the management of bronchial asthma in paediatric and adult age group for primary health care doctors giving them up-to-date guidelines and treatment protocols. Another important application was developed by Wallis, Fleming, Hasselberg, Laflamme, and Lundin (2016) that supported medical decision making through standard guidelines to manage burned patients. Such mHealth applications could reduce the number of unintended treatment errors and guide the medical professionals towards the standard protocols.
mHealth Applications as a Shift for Healthcare Management
Literature suggests that there are number mHealth applications that are readily available for people to use them. This is evident in consumers’ dependency on mHealth applications in receiving information about their health conditions and healthcare professionals’ increase of using them to provide health services thorough these applications (Lupton & Jutel, 2015). Many researchers (Michie, Yardley, West, Patrick, & Greaves, 2017; Owolabi, Odugbemi, Odeyemi, & Onigbogi, 2018; Varshney, 2014) suggest that mHealth applications have potential to revolutionise the way healthcare is provided in many ways: (1) more personalised care can be tailored for specific customers/patients through direct communication between them and health professionals, (2) interactive, reliable, authentic applications can empower patients who are technology-friendly, (3) mHealth applications can have access to public health information system who can provide useful alerts and advices towards better health management and quality life and (4) mHealth applications can provide health and fitness programmes with personalised features suggesting healthy diets, advanced muscle building and healthy life style advices.
Conclusion
The reviewed literature identified that mHealth applications can support medical decision making for both healthcare providers and patients by providing authentic medical information and standard guidelines. These applications can empower patients’ active involvement in their health-related decision, making them partners in their decision making for critical health-related decisions. However, the literature noted that lack of or absence of unified standards in health-related information encompassed with mHealth applications could create some difficulties to healthcare providers, as patients may likely to be convinced with the information they receive through these applications prior to their doctor’s consultations. This paper recommends streamline of medical references and knowledge bases in the content of mHealth applications to increase the authenticity and reliability of mHealth applications.
References
Abbasgholizadeh Rahimi, S., Menear, M., Robitaille, H., & Légaré, F. (2017). Are mobile health applications useful for supporting shared decision making in diagnostic and treatment decisions? Global health action, 10(sup3), 1332259.
Albuquerque, S. L., & Gondim, P. R. (2016). Security in cloud-computing-based mobile health. IT Professional, 18(3), 37-44.
Anand, V., & Spalding, S. J. (2015). Leveraging Electronic Tablets and a Readily Available Data Capture Platform to Assess Chronic Pain in Children: The PROBE system. Stud Health Technol Inform, 216, 554-558.
Arroyo-Gallego, T., Ledesma-Carbayo, M. J., Sanchez-Ferro, A., Butterworth, I., Mendoza, C. S., Matarazzo, M., Giancardo, L. (2017). Detection of Motor Impairment in Parkinson's Disease Via Mobile Touchscreen Typing. IEEE Trans Biomed Eng, 64(9), 1994-2002. doi:10.1109/tbme.2017.2664802.
Bakibinga, P., Kamande, E., Omuya, M., Ziraba, A. K., & Kyobutungi, C. (2017). The role of a decision-support smartphone application in enhancing community health volunteers' effectiveness to improve maternal and newborn outcomes in Nairobi, Kenya: quasi-experimental research protocol. BMJ open, 7(7), e014896. doi:10.1136/bmjopen-2016-014896.
Bansal, A., Kumar, S., Bajpai, A., Tiwari, V. N., Nayak, M., Venkatesan, S., & Narayanan, R. (2015). Remote health monitoring system for detecting cardiac disorders. IET Syst Biol, 9(6), 309-314. doi:10.1049/iet-syb.2015.0012.
Bradway, M., Årsand, E., & Grøttland, A. (2015). Mobile Health: Empowering patients and driving change. Trends in Endocrinology & Metabolism, 26(3), 114-117.
Charani, E., Gharbi, M., Moore, L. S. P., Castro-Sanchez, E., Lawson, W., Gilchrist, M., & Holmes, A. H. (2017). Effect of adding a mobile health intervention to a multimodal antimicrobial stewardship programme across three teaching hospitals: an interrupted time series study. J Antimicrob Chemother, 72(6), 1825-1831. doi:10.1093/jac/dkx040.
Dafli, E., Antoniou, P., Ioannidis, L., Dombros, N., Topps, D., & Bamidis, P. D. (2015). Virtual patients on the semantic Web: a proof-of-application study. J Med Internet Res, 17(1), e16. doi:10.2196/jmir.3933.
Dicianno, B. E., Parmanto, B., Fairman, A. D., Crytzer, T. M., Yu, D. X., Pramana, G., Petrazzi, A. A. (2015). Perspectives on the Evolution of Mobile (mHealth) Technologies and Application to Rehabilitation. Physical therapy, 95(3), 397-405. doi:10.2522/ptj.20130534.
Dunsmuir, D. T., Payne, B. A., Cloete, G., Petersen, C. L., Gorges, M., Lim, J., Ansermino, J. M. (2014). Development of mHealth applications for pre-eclampsia triage. IEEE J Biomed Health Inform, 18(6), 1857-1864. doi:10.1109/jbhi.2014.2301156
Elwyn, G., Frosch, D., Thomson, R., Joseph-Williams, N., Lloyd, A., Kinnersley, P., Rollnick, S. (2012). Shared decision making: a model for clinical practice. Journal of general internal medicine, 27(10), 1361-1367.
Evans, K. H., Daines, W., Tsui, J., Strehlow, M., Maggio, P., & Shieh, L. (2015). Septris: a novel, mobile, online, simulation game that improves sepsis recognition and management. Acad Med, 90(2), 180-184. doi:10.1097/acm.0000000000000611
Frandes, M., Timar, B., Tole, A., Holban, S., & Lungeanu, D. (2015). Mobile technology support for clinical decision in diabetic keto-acidosis emergency. Stud Health Technol Inform, 210, 316-320.
Gulayin, P., Irazola, V., Lozada, A., Chaparro, M., Santero, M., Gutierrez, L., Rubinstein, A. (2017). Educational intervention to improve effectiveness in treatment and control of patients with high cardiovascular risk in low-resource settings in Argentina: study protocol of a cluster randomised controlled trial. BMJ open, 7(1), e014420. doi:10.1136/bmjopen-2016-014420.
Guo, Y., Chen, Y., Lane, D. A., Liu, L., Wang, Y., & Lip, G. Y. H. (2017). Mobile Health Technology for Atrial Fibrillation Management Integrating Decision Support, Education, and Patient Involvement: mAF App Trial. Am J Med, 130(12), 1388-1396.e1386. doi:10.1016/j.amjmed.2017.07.003.
Hagberg, H., Siebert, J., Gervaix, A., Daehne, P., Lovis, C., Manzano, S., & Ehrler, F. (2016). Improving Drugs Administration Safety in Pediatric Resuscitation Using Mobile Technology. Stud Health Technol Inform, 225, 656-657.
Hoff, B. M., Ford, D. C., Ince, D., Ernst, E. J., Livorsi, D. J., Heintz, B. H., Ford, B. A. (2018). Implementation of a Mobile Clinical Decision Support Application to Augment Local Antimicrobial Stewardship. J Pathol Inform, 9, 10. doi:10.4103/jpi.jpi_77_17.
Hsu, J. M. (2015). Digital health technology and trauma: development of an app to standardize care. ANZ J Surg, 85(4), 235-239. doi:10.1111/ans.12945
Huang, R. S., Nedelcu, E., Bai, Y., Wahed, A., Klein, K., Gregoric, I., Nguyen, A. N. (2014). Mobile computing platform with decision support modules for hemotherapy. Am J Clin Pathol, 141(6), 834-840. doi:10.1309/ajcprg5lywl6dxmx.
Joseph-Williams, N., Elwyn, G., & Edwards, A. (2014). Knowledge is not power for patients: a systematic review and thematic synthesis of patient-reported barriers and facilitators to shared decision making. Patient education and counseling, 94(3), 291-309.
Kaneez, S., & Hassan, M. (2015). Information technology in medicine. JK-Practitioner, 20(1-2), 47-48.
Kay, M., Santos, J., & Takane, M. (2011). mHealth: New horizons for health through mobile technologies. World Health Organization, 64(7), 66-71.
Knoble, S. J., & Bhusal, M. R. (2015). Electronic diagnostic algorithms to assist mid-level health care workers in Nepal: a mixed-method exploratory study. Int J Med Inform, 84(5), 334-340. doi:10.1016/j.ijmedinf.2015.01.011.
Lamprinos, I., Demski, H., Mantwill, S., Kabak, Y., Hildebrand, C., & Ploessnig, M. (2016). Modular ICT-based patient empowerment framework for self-management of diabetes: Design perspectives and validation results. Int J Med Inform, 91, 31-43. doi:10.1016/j.ijmedinf.2016.04.006.
Lang, M., & Zawati, M. n. H. (2018). The app will see you now: mobile health, diagnosis, and the practice of medicine in Quebec and Ontario. Journal of Law and the Biosciences, 5(1), 142-173.
Légaré, F., Stacey, D., Turcotte, S., Cossi, M. J., Kryworuchko, J., Graham, I. D., Elwyn, G. (2014). Interventions for improving the adoption of shared decision making by healthcare professionals. The Cochrane Library.
Légaré, F., & Witteman, H. O. (2013). Shared decision making: examining key elements and barriers to adoption into routine clinical practice. Health Affairs, 32(2), 276-284.
Lloyd, B., Groat, D., Cook, C. B., Kaufman, D., & Grando, A. (2015). iDECIDE: A Mobile Application for Insulin Dosing Using an Evidence Based Equation to Account for Patient Preferences. Stud Health Technol Inform, 216, 93-97.
Lopez-Guede, J. M., Moreno-Fernandez-de-Leceta, A., Martinez-Garcia, A., & Grana, M. (2015). Lynx: Automatic Elderly Behavior Prediction in Home Telecare. Biomed Res Int, 2015, 201939. doi:10.1155/2015/201939.
Lopez, M. M., Lopez, M. M., de la Torre Diez, I., Jimeno, J. C. P., & Lopez-Coronado, M. (2017). mHealth App for iOS to Help in Diagnostic Decision in Ophthalmology to Primary Care Physicians. J Med Syst, 41(5), 81. doi:10.1007/s10916-017-0731-6
Losiouk, E., Lanzola, G., Visetti, E., & Quaglini, S. (2015). An environment for representing and using medical checklists on mobile devices. Conf Proc IEEE Eng Med Biol Soc, 2015, 7328-7331. doi:10.1109/embc.2015.7320084.
Losiouk, E., Quaglini, S., Pesenti Campagnoni, M., & Lanzola, G. (2015). A mobile platform for emergency care. Stud Health Technol Inform, 210, 818-822.
Lupton, D., & Jutel, A. (2015). ‘It's like having a physician in your pocket!’A critical analysis of self-diagnosis smartphone apps. Social Science & Medicine, 133, 128-135.
MacWalter, G., McKay, J., & Bowie, P. (2016). Utilisation of internet resources for continuing professional development: a cross-sectional survey of general practitioners in Scotland. BMC medical education, 16(1), 24.
Manaktala, S., & Claypool, S. R. (2017). Evaluating the impact of a computerized surveillance algorithm and decision support system on sepsis mortality. J Am Med Inform Assoc, 24(1), 88-95. doi:10.1093/jamia/ocw056.
Maulik, P. K., Kallakuri, S., Devarapalli, S., Vadlamani, V. K., Jha, V., & Patel, A. (2017). Increasing use of mental health services in remote areas using mobile technology: a pre-post evaluation of the SMART Mental Health project in rural India. J Glob Health, 7(1), 010408. doi:10.7189/jogh.07.010408.
Maulik, P. K., Tewari, A., Devarapalli, S., Kallakuri, S., & Patel, A. (2016). The Systematic Medical Appraisal, Referral and Treatment (SMART) Mental Health Project: Development and Testing of Electronic Decision Support System and Formative Research to Understand Perceptions about Mental Health in Rural India. PLOS ONE, 11(10), e0164404. doi:10.1371/journal.pone.0164404.
McRae, M. P., Simmons, G., Wong, J., & McDevitt, J. T. (2016). Programmable Bio-nanochip Platform: A Point-of-Care Biosensor System with the Capacity To Learn. Acc Chem Res, 49(7), 1359-1368. doi:10.1021/acs.accounts.6b00112
Menezes, J., Jr., & Gusmao, C. (2015). Development of a Mobile System Decision-support for Medical Diagnosis of Asthma in Primary Healthcare--InteliMED. Stud Health Technol Inform, 216, 959.
Meyer, A. N. D., Thompson, P. J., Khanna, A., Desai, S., Mathews, B. K., Yousef, E., Singh, H. (2018). Evaluating a mobile application for improving clinical laboratory test ordering and diagnosis. J Am Med Inform Assoc. doi:10.1093/jamia/ocy026.
Michie, S., Yardley, L., West, R., Patrick, K., & Greaves, F. (2017). Developing and evaluating digital interventions to promote behavior change in health and health care: recommendations resulting from an international workshop. Journal of Medical Internet Research, 19(6).
O'Donovan, J., Bersin, A., & O'Donovan, C. (2015). The effectiveness of mobile health (mHealth) technologies to train healthcare professionals in developing countries: a review of the literature. BMJ Innovations, 1(1), 33-36.
Owolabi, B. S., Odugbemi, T. O., Odeyemi, K. A., & Onigbogi, O. O. (2018). mHealth: Knowledge and use among doctors and nurses in public secondary health-care facilities of Lagos, Nigeria. Journal of Clinical Sciences, 15(1), 27.
Park, J., Lee, K., & Kang, K. (2015). Pit-a-Pat: A Smart Electrocardiogram System for Detecting Arrhythmia. Telemed J E Health, 21(10), 814-821. doi:10.1089/tmj.2014.0187.
Patzer, R. E., Basu, M., Larsen, C. P., Pastan, S. O., Mohan, S., Patzer, M., . . . Arriola, K. J. (2016). iChoose Kidney: A Clinical Decision Aid for Kidney Transplantation Versus Dialysis Treatment. Transplantation, 100(3), 630-639. doi:10.1097/tp.0000000000001019.
Payne, K. F., Weeks, L., & Dunning, P. (2014). A mixed methods pilot study to investigate the impact of a hospital-specific iPhone application (iTreat) within a British junior doctor cohort. Health Informatics J, 20(1), 59-73. doi:10.1177/1460458213478812.
Pezzin, L. E., Laud, P., Neuner, J., Yen, T. W., & Nattinger, A. B. (2016). A statewide controlled trial intervention to reduce use of unproven or ineffective breast cancer care. Contemp Clin Trials, 50, 150-156. doi:10.1016/j.cct.2016.08.005.
Prinja, S., Nimesh, R., Gupta, A., Bahuguna, P., Thakur, J. S., Gupta, M., & Singh, T. (2016). Impact assessment and cost-effectiveness of m-health application used by community health workers for maternal, newborn and child health care services in rural Uttar Pradesh, India: a study protocol. Glob Health Action, 9, 31473. doi:10.3402/gha.v9.31473.
Raghu, A., Praveen, D., Peiris, D., Tarassenko, L., & Clifford, G. (2015). Engineering a mobile health tool for resource-poor settings to assess and manage cardiovascular disease risk: SMARThealth study. BMC Med Inform Decis Mak, 15, 36. doi:10.1186/s12911-015-0148-4.
Ramirez, M., Wu, S., Ryan, G., Towfighi, A., & Vickrey, B. G. (2017). Using Beta-Version mHealth Technology for Team-Based Care Management to Support Stroke Prevention: An Assessment of Utility and Challenges. JMIR Res Protoc, 6(5), e94. doi:10.2196/resprot.7106.
Sa, J. H., Rebelo, M. S., Brentani, A., Grisi, S. J., Iwaya, L. H., Simplicio, M. A., Jr., Gutierrez, M. A. (2016). Georeferenced and secure mobile health system for large scale data collection in primary care. Int J Med Inform, 94, 91-99. doi:10.1016/j.ijmedinf.2016.06.013.
Sarwar, M., & Soomro, T. R. (2013). Impact of Smartphone’s on Society. European journal of scientific research, 98(2), 216-226.
Sheats, J. L., Winter, S. J., Romero, P. P., & King, A. C. (2017). FEAST: Empowering Community Residents to Use Technology to Assess and Advocate for Healthy Food Environments. J Urban Health, 94(2), 180-189. doi:10.1007/s11524-017-0141-6.
Singler, K., Roth, T., Beck, S., Cunningham, M., & Gosch, M. (2016). Development and initial evaluation of a point-of-care educational app on medical topics in orthogeriatrics. Arch Orthop Trauma Surg, 136(1), 65-73. doi:10.1007/s00402-015-2366-8.
Statista. (2018, 2018). Number of Mobile phone users Worldwide from 2013 to 2019 (in billions). Retrieved from https://www.statista.com/statistics/274774/forecast-of-mobile-phone-users-worldwide/.
Steinhubl, S. R., Muse, E. D., & Topol, E. J. (2015). The emerging field of mobile health. Science translational medicine, 7(283), 283rv283-283rv283.
Timbi-Sisalima, C., Rodas, E. B., Salamea, J. C., Sacoto, H., Monje-Ortega, D., & Robles-Bykbaev, V. (2015). An Intelligent Ecosystem for Providing Support in Prehospital Trauma Care in Cuenca, Ecuador. Stud Health Technol Inform, 216, 329-332.
Trevisonno, M., Kaneva, P., Watanabe, Y., Fried, G., Feldman, L., Lebedeva, E., & Vassiliou, M. (2015). A survey of general surgeons regarding laparoscopic inguinal hernia repair: practice patterns, barriers, and educational needs. Hernia, 19(5), 719-724.
Tshiamo, W. B., Kgositau, M., & Magowe, M. (2017). Use of Information and Communication Technology by Health Care Providers for Continuing Professional Development in Botswana. In Health Information Systems and the Advancement of Medical Practice in Developing Countries (pp. 181-192): IGI Global.
van Os, J., Verhagen, S., Marsman, A., Peeters, F., Bak, M., Marcelis, M., Delespaul, P. (2017). The experience sampling method as an mHealth tool to support self-monitoring, self-insight, and personalized health care in clinical practice. Depress Anxiety, 34(6), 481-493. doi:10.1002/da.22647.
Varshney, U. (2014). Mobile health: Four emerging themes of research. Decision Support Systems, 66, 20-35.
Ventola, C. L. (2014). Mobile Devices and Apps for Health Care Professionals: Uses and Benefits. Pharmacy and Therapeutics, 39(5), 356-364.
Wallis, L. A., Fleming, J., Hasselberg, M., Laflamme, L., & Lundin, J. (2016). A Smartphone App and Cloud-Based Consultation System for Burn Injury Emergency Care. PLOS ONE, 11(2), e0147253. doi:10.1371/journal.pone.0147253.
Wang, D., Xiang, Z., & Fesenmaier, D. R. (2016). Smartphone Use in Everyday Life and Travel. Journal of Travel Research, 55(1), 52-63. doi:10.1177/0047287514535847
Warner, J. L., Denny, J. C., Kreda, D. A., & Alterovitz, G. (2015). Seeing the forest through the trees: uncovering phenomic complexity through interactive network visualization. J Am Med Inform Assoc, 22(2), 324-329. doi:10.1136/amiajnl-2014-002965.
Whelan, P., Machin, M., Lewis, S., Buchan, I., Sanders, C., Applegate, E., Ainsworth, J. (2015). Mobile early detection and connected intervention to coproduce better care in severe mental illness. Stud Health Technol Inform, 216, 123-126.
Wolf, S. L., Kwakkel, G., Bayley, M., & McDonnell, M. N. (2016). Best practice for arm recovery post stroke: an international application. Physiotherapy, 102(1), 1-4. doi:10.1016/j.physio.2015.08.007.
Yang, F., Ji, M., Ding, S., Wu, Y., Chang, P., Lin, C., & Yang, X. (2016). The Development and Evaluation of Delirium Assessment and Nursing Care Decision-Making Assistant Mobile Application for Intensive Care Unit. Stud Health Technol Inform, 225, 668-672.

Comments
No comments